Image Credit: https://www.divein.com/ / Edited with Photoshop
My last two blog posts tackled astigmatism in detail and touched base with keratoconus. I recently had an eye check up with my doctor. He was concerned that I may have keratoconus because my astigmatism was so high. That's why he asked me to have a comprehensive eye exam. Fortunately, it was a false alarm. That, however, prompted me to learn more about this eye condition. So, what exactly is keratoconus and why is it important to detect and treat this eye condition as early as possible?
What is Keratoconus?
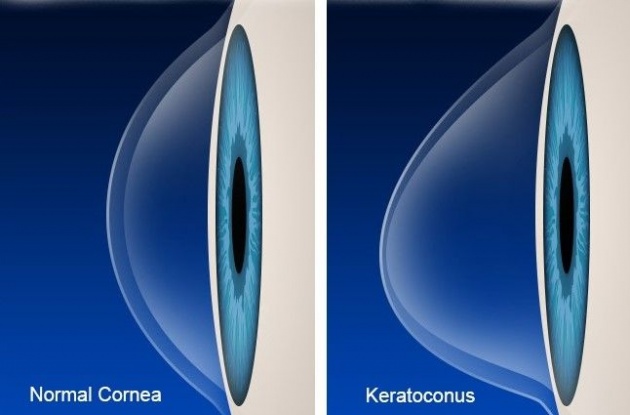
Image Credit: https://3dprintingindustry.com/
The cornea of the eye is normally round and dome-shaped. However, people with keratoconus have more like a cone-shaped cornea. This happens because the cornea becomes so thin and stretched near the center that it bulges forward causing it to distort into a conical shape.
The cornea is the clear surface at the front of the eyeball. It refracts the light entering the eye onto the lens, which then focuses it onto the retina.
Source: www.lei.org.au/
It is a progressive eye disease that usually affects both eyes. However, the degree of progression in each eye may differ. Oftentimes, the disease will be more advanced in just one eye. Keratoconus does not cause total vision loss, but it can still lead to significant vision impairment, especially if left untreated.
Here's a visual representation of what keratoconus actually is.
Video Credit: sassyautumn via Youtube
Causes
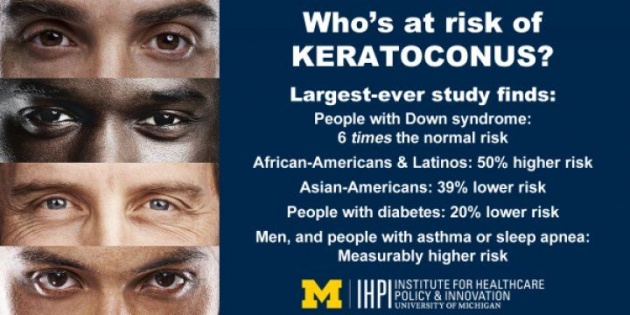
Image Credit: https://www.sciencedaily.com/
No one knows the exact cause of keratoconus, but certain factors can increase your risk of developing one. Such keratoconus risk factors include genetics and certain medical conditions such as:
Excessive and vigorous rubbing of the eyes may also increase your risk factor.
Signs and Symptoms

Image credit: https://www.opticalmasters.com/
As the disease progress, the signs and symptoms of keratoconus may change. Keratoconus usually starts as being just an irregularity in the shape of the cornea. At this point, you probably won't be showing any symptoms yet. But as the shape of the cornea starts to take a more conical shape, you will begin to notice changes in your vision.
The most common ones include the following.
- Blurred or distorted vision
- Increased sensitivity to glare and bright light which can be problematic when driving at night
- Sudden clouding or worsening of vision
You may also need to have a constant change in eyeglass prescriptions depending on the progress of the disease.
Complications
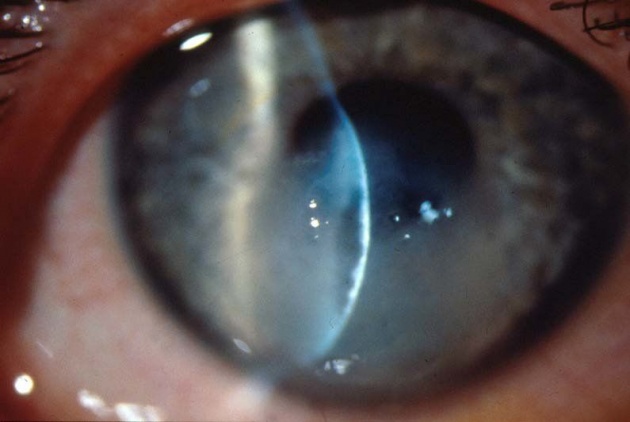
Image CreditL: https://www.researchgate.net/
In some cases, your cornea can swell quickly, causing sudden vision impairment, as well as scarring of the cornea. This may be caused by corneal hydrops where the inside lining of the cornea breaks down which allows water to enter the cornea. Corneal hydrops, or corneal rupture, is a rare complication of keratoconus. It is mostly seen in people with advanced stages of keratoconus or other corneal ectatic disorders. Another complication that comes with advanced keratoconus is scarring of the cornea, which may require corneal transplant surgery to avoid worsening vision problems.
Diagnosis
To check if you have keratoconus, your eye doctor will conduct a thorough review of your medical and family history. You will also need to undergo a comprehensive eye exam. Your eye doctor may also require that you go through other tests to determine the shape of your eye.
The common tests for diagnosing keratoconus include the following.
Eye refraction
Your eye doctor will check for vision problems with the use of a special equipment that measures your eyes. He or she may instruct you to peer through a device called phoropter which contains wheels of different lenses. This will help your doctor judge which combination provides you with the sharpest vision. in some instances, your doctor may also use a handheld device called retinoscope to help evaluate your eyes.
Slit-lamp examination
In this eye test, a vertical beam of light is directed on the surface of the eye. Your doctor will also use a low-powered microscope to peer into your eye. He or she will then evaluate the shape of the cornea and look for other possible problems in your eye. The test may be repeated after eyedrops have been applied to your eye to dilate the pupil. This will help your doctor view the back of your eye.
Keratometry
In this test, your eye doctor is able to determine the shape of your cornea by focusing a circle of light into your eyes and measuring its reflection.
Computerized corneal mapping
Optical coherence tomography and corneal topography are types of special photographic tests that record images of the cornea in order to create a detailed map of the shape of the cornea's surface. They can also be used to determine and measure the thickness of the cornea.
Treatments
Keratoconus treatments vary depending on the severity of your eye condition and the speed at which it is progressing. Treatment for mild to moderate keratoconus includes the use of contact lenses or eyeglasses. In most cases, this treatment is enough to strengthen the cornea over time. If this is you, you are in luck because it's highly likely that you won't experience severe vision problems or need further treatment.
However, if you have a more severe case of keratoconus where the cornea becomes scarred, it will make wearing contact lenses extra difficult. Patients with such cases may need to undergo surgery.
Some of the most common keratoconus treatments include the following.
Lenses

Image Credit: https://www.coastal.com/
Most of us are familiar with only two types of lenses which are eyeglasses and contact lenses. However, there are several other varieties to them, such as the following.
- Eyeglasses
- Soft contact lenses
- Hard contact lenses
- Piggyback lenses
- Hybrid lenses
- Scleral lenses
Rigid and scleral lenses need to be fitted by a qualified eye doctor who has a vast experience in treating keratoconus. You also need to have regular checkups to ensure that your lenses are still fitted correctly. Ill-fitting lenses can damage the cornea of your eyes.
Surgery
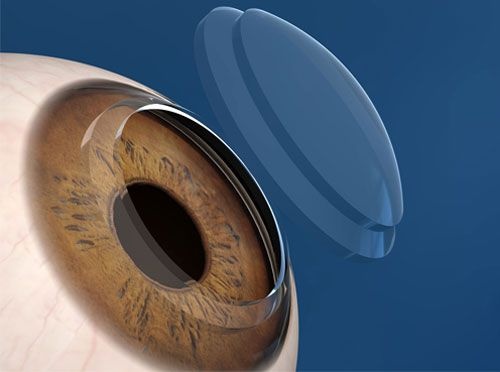
Image Credit: eyecenterofmidland.com/
If you have any of the following, your doctor will most likely recommend you to have surgery.
- Corneal scarring
- Thinning of the cornea
- Poor vision even with the use of the strongest prescription lenses
- Inability to tolerate the use of any type of contact lenses.
There are several surgical options available for you depending on the severity of your condition and the location of the bulging cone. Your options include:
Of course, just like with any other type of surgery, these eye surgeries also carry some risks and possible complications. Your doctor should be able to explain these risks and complications in detail to you.
Concluding Thoughts
Keratoconus is a less common eye condition than astigmatism but many people still suffer from. Some of them may not even be aware that they have it--which is quite alarming since this degenerative eye disease progresses faster in younger patients. This is the reason why early detection is so important. If you have reason to believe that your eyesight has changed or it's not as it used to be, don't hesitate to visit the local ophthalmologist.
~~oO0Oo~~oO0Oo~~oO0Oo~~
Thanks for reading! Have a wonderful day ahead of you and keep smiling. :)
Written by Chineyes for bitLanders
For more quality blog posts, you may visit my page
Not yet on bitLanders? Sign up now and be rewarded for sharing ideas, photos, and videos!