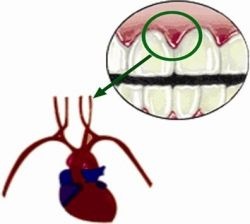
Association of oral and systemic diseases has gained importance due to the high incidence of oral disease is a very common source of infection. Epidemiological studies have periodontal diseases presented as a risk factor for developing cardiovascular diseases. A chronic oral infections such as periodontitis is a potential source of constant infection and is now considered an independent risk factor for cardiovascular disease, cerebrovascular disease, peripheral arterial disease and respiratory diseases, as well as the delivery of children with low birthweight born. The possible pathways linking oral infections are systemic metastatic disease, bacterial endotoxins, and systemic vascular injury. People with a history of periodontal disease and / or tooth loss are at increased risk of peripheral arterial disease (PAD) compared to those without periodontal disease and / or tooth loss. All studies on the relationship between periodontal disease to cardiovascular disease are inconclusive and most data are based on epidemiological studies.

Epidemiological studies have periodontal diseases presented as a risk factor for developing cardiovascular diseases. The association between oral infection and systemic diseases is not new. Chronic oral infections such as periodontal diseases are a constant potential source of infection. The oral cavity and oropharynx have been described as a "system of open mouth" for bacteria and other organisms that adhere to both shedding (soft tissue) and non-shedding (teeth, restorations, dentures) surfaces. The mouth serves as a mirror of health or disease, as an essential early warning system or as an accessible model for the study of other tissues and organs and as a potential source of pathology that affects other systems and organs. The most common diseases of the oral cavity are dental caries and periodontal diseases and measures of oral health status are taken. Periodontitis, periapical lesions, pericoronitis and abscesses are possible sources of infection in the oral cavity. Many systemic diseases such as diabetes mellitus, cardiovascular diseases, respiratory diseases and infants of low birth weight are related to oral infections. More recent epidemiological studies have reported periodontal disease as a risk factor for development of cardiovascular (CHD), cerebrovascular disease (stroke) and peripheral arterial disease (PAD) and this relationship has been reviewed here.
Oral infection Association of systemic diseases
Herzberg cited the Assyrians who proposed the effect of oral health in the rest of the body and in the seventh century BC "theory of focal infection" was published in 1891 suggests that microorganisms or their waste products gain entry to the parties body adjacent to or remote from the point of entry. Other proponents of this theory oral foci of infection blamed for a series of regional and systemic diseases, ranging from tonsillitis and middle ear infections, pneumonia, tuberculosis, syphilis, osteomyelitis, endocarditis, meningitis and septicemia. The "theory of focal infection" was not given any attention until recent advances in the identification and characterization of periodontal pathogens and clarify the possible systemic mechanisms of action of bacterial products and inflammatory cytokines. This has opened the way for a more realistic assessment of the systemic importance of periodontal disease. Studies have given credence to the idea that periodontal disease may be an independent risk factor for cardiovascular disease, cerebrovascular disease and respiratory disease, as well as the delivery of children with low birth weight. However, it is important that oral infections are often just one of the many confounding factors that may influence systemic diseases.
Periodontal diseases
Periodontal diseases have prevailed throughout human history, but without the obvious secular variations. Research and clinical trials indicate that the damage to the supporting structures of the teeth due to periodontal disease in adult life is irreparable, whereas in adulthood media destroys much of the natural dentition and deprives many people of all teeth long before old age. The effects of periodontal disease in the general health of the population are in-
Periodontal diseases
evaluable. Inflammatory periodontal diseases are probably the most common infections in the world. Gingivitis is present in the vast majority of adults worldwide, but is more pronounced in developing countries. Moderate periodontitis affects approximately 30 percent and advanced periodontitis about 10pc of US adult populations .. Deep pockets are present in 2-18pc of adults in Western countries and more prevalent in developing countries .
Periodontal disease is currently believed to progress in newspapers, relatively short rapid tissue destruction episodes. Some people have frequent episodes of active disease in many places in the mouth, while others experience much less active disease with signs of gingivitis and may be some pockets but no insertion loss over long periods. His initiation and progression is influenced by a wide variety of determinants and factors, including characteristics of the subjects, social and behavioral factors, systemic factors, genetic factors, factors -level teeth, microbial composition of plaque and other emerging factors . Because gum disease is common in populations may represent a significant part of the risk associated with infection proposal CVD. Interestingly, periodontal diseases share a number of characteristics; old age, smoking, low education status, diabetes and stress, all common cardiovascular disease.
Cardiovascular Diseases
Cardiovascular diseases (CVD) are the most frequent category of systemic diseases in countries, developed and developing countries are increasing age.14
Statistics from the World Health Organization in 1995 indicated that cardiovascular diseases accounted for 20pc of deaths worldwide and in some developing countries accounted for 50pc of deaths.15 CVD contributed to a third of all deaths worldwide . Low- and middle-income accounted for 78pc of CVD deaths in 1999. By 2010 CVD is estimated to be the leading cause of death in developing countries.
1. Periodontal disease and cerebrovascular disease: cerebrovascular accident
The relationship of periodontal disease for ischemic stroke has been evaluated in several studies. The result is different from the reported studies, ranging from total distance of fatal stroke, non-fatal stroke and ischemic stroke. The study by Beck and colleagues compared men who had some kind of stroke with men who did not develop cardiovascular disease during follow-up. They found a significant association between periodontal disease and total stroke: relative risk (RR) of 2.80.5 Wu and his colleagues found a possible association between periodontal disease and ischemic stroke (RR = 2.11); the risk was even greater when restricted to a fatal stroke. Although studies have shown an association between tooth loss and periodontal disease and stroke, no two studies are consistent in defining outcomes and exposure. Therefore, no association has been truly replicated. It is difficult to rule out residual confounding variables, as there are several common risk factors.
2. Periodontal disease and coronary artery disease
Periodontal disease is a chronic infection and may be associated with systemic inflammatory conditions. A number of studies provides a data set to statistically significant and suggest and support the relationship of periodontal disease to cardiovascular disease. The majority of risk factors for cardiovascular disease are also considered risk factors for periodontal disease.
Mattila et al suggested a statistical association between the severity of coronary stenosis and dental infections. The data support the hypothesis that oral infections can play a role in the development of adverse cardiovascular outcomes. Studies by Beck et al and Arbes et al also provide some support for the hypothesis that periodontal disease and tooth loss could play a role in the development of CHD. However, the likelihood of residual considerable confusion remains there in all these studies. Hujoel et al presented a negative association between periodontal disease and coronary heart disease in later first national longitudinal study of health and Nutrition Examination Surveys (NHANES-I) with 21 years of follow up.
Periodontal disease and peripheral arterial disease
PAD shares one common underlying pathological change, atherosclerosis, coronary heart disease and stroke. Very few studies have reported on the relationship of periodontal disease to PAD.
In a cohort study of 51,529 health professionals including 29,683 dentists 40-75 years conducted between 1986 and 1998, tooth loss and periodontal disease experience was recorded through biennial self reported questionnaires. A total of 342 cases of PAD (255 definite and 87 probable) were recorded. In this era multivariate model, smoking, alcohol, family history of myocardial infarction, use of supplemental multivitamins, vitamin E intake, history of hypertension, diabetes, hypercholesterolemia and profession (dentist / non-dentist) is adjusted and updated based on biennial questionnaires. Periodontal disease is also taken as a causative factor in tooth loss. The study concluded that men with a history of periodontal disease or tooth loss during follow-up had a significantly higher risk of PAD than men without periodontitis or without any loss of teeth. Incident tooth loss was significantly associated with PAD, especially among men with periodontal disease. In a follow-up study of 1,030 subjects 25-30 years Mendez et al reported that subjects with clinically significant at baseline periodontal disease had a relative risk of 2.27 of having PAD.
The relationship of periodontal disease to cardiovascular disease - Literature Review
Mechanism proposed periodontal infection and association CHD / Stroke.
Infection has been recognized as a risk factor of atherogenesis and thromboembolic events. Gram-negative bacteria or associated lipopolysacchride (endotoxin), when present as a systemic challenge in animal models, can induce inflammatory cell infiltration in the major blood vessels, proliferation of vascular smooth muscle, vascular fatty degeneration and intravascular coagulation. The remarkable similarities of bacterial-induced vascular disease, natural history of atherogenesis has led some researchers to suggest that in addition to genetics, lifestyle and dietary influences, unexplained infections can contribute to cardiovascular disease observed. The burden of chronic inflammatory periodontal infection and the host response provided the basis for our hypothetical model of the observed associations between periodontal disease and atherosclerosis, coronary heart disease and stroke. This model emphasizes that among certain individuals may be an underlying hyperinflammatory feature in response to stimuli is manifested by excessive production of proinflammatory cytokines and lipid mediators by monocytes and other cell types. Four possible mechanisms by which periodontal infections can contribute to the pathogenesis of heart disease and stroke have gained importance and these include effects of endotoxin in circulation, the role of heat shock proteins, perturbations induced by infection in lipid profiles and training of acute phase reactants.
1. Effects of endotoxin in circulation
Microflora associated with periodontal infections is a rich source of endotoxins, which are lipopolysacchride (LPS) components of the cell walls of all gram-negative bacteria. Check endotoxin in the circulation can occur from many sources, including respiratory infections (C. Pneumonae), gastric ulcers (H. pylori) and periodontitis (P. gingivalis, Actinobacillus A., B. forsythus, etc). Once you enter the circulation endotoxins that pose a significant threat to the welfare of the host. They can directly damage endothelial cells, promote adhesion of mono- cytes to endothelial formation25 induce macrophage foam cells, and generally cause endothelial dysfunction. All these effects play a significant role in the initiation and development of atherosclerosis. One of the main characteristics of acute occlusion of vessels in heart disease and stroke are the disruption of atherosclerotic plaques existing inflammation mediated by macrophages.
2. Role of heat shock proteins
Heat shock proteins (HSP) are produced by a wide variety of bacteria and human cells under a variety of stress or harsh conditions such as high temperature, infection, inflammation and mechanical stress. It is well established that endothelial cells produce Hsp under stress conditions such as exposure to endotoxins.
3. perturbations induced by infection in lipid profiles
It is known from studies hyperlipidemia often accompanies many bacterial infections. Low doses of endotoxin causes a rapid rise in serum triglycerides due to an increase in lipoprotein rich very low density triglyceride (VLDL). Hyperlipidemia can have negative effects, such as promoting the release of proinflammatory cytokines from neutrophils. Interestingly, hyperlipidemia occurs during periodontal infections. Cytokines such as IL-I, IL-6 and TNF have been implicated as risk factors for heart disease and prolonged hyperlipidemia is likely to have adverse clinical effects.
4. Formation of acute phase reactants
Acute phase reactants appear in the circulation in response to tissue infection and injury. C-reactive protein (CRP) is of particular interest since in the levels of "high" -Normal has proven to be an important risk factor for CHD and is also elevated in patients with extensive periodontal disease. Remains whether elevations occurring during PCR periodontal infections play a role in atherosclerosis.
Conclusions and Recommendations
The results of epidemiological studies on the relationship of periodontal disease to cardiovascular disease are inconsistent and lead to the conservative conclusion. The studies do not prove a causal relationship and not the present periodontal disease in weak association as one of the confounders. Studies show a lack of control for confounders, residual confounding factors, as well as control of the cofounders. Although both periodontal and cardiovascular diseases share biological potential risk factors (diabetes) and behavioral risk factors (diet, snuff, etc.), the link between periodontal disease and cardiovascular problems is weak and is a difficult task demonstrate the role of periodontal disease in the etiology of cardiovascular diseases. Intervention studies are needed to understand the role of periodontal disease in the initiation and progression of cardiovascular disease. Longitudinal and case-control to locate the association of both diseases with well-controlled confounding factors and outcomes for periodontal disease studies are also needed.



